While the fiscal year (FY) 2014 budget proposal shows higher funding levels for most of the District’s health care programs, the Healthcare Alliance faces its second consecutive cut as enrollment in the program continues to decline. The Alliance program provides basic health coverage for uninsured District residents who have incomes below 200 percent of the federal poverty line but do not qualify for Medicaid. Since the implementation of a six-month, face-to-face recertification process for Alliance participants, enrollment in the Alliance has declined significantly. The rapid decline suggests that this restrictive process is creating hurdles for eligible residents and is overburdening the DC government staff in charge of administering the policy. 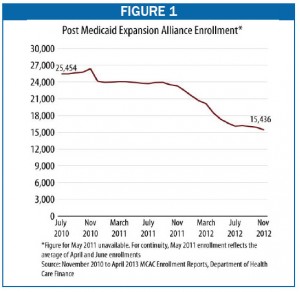
For FY 2014, the Department of Healthcare Finance’s proposed budget provides $40 million for Alliance provider payments, a cut of $2 million, or 5 percent, over the FY 2013 budget after adjusting for inflation. The cut corresponds with a decline in enrollment ‘ from 24,000 enrollees in September of 2011 to 15,400 in November ‘ that began with the implementation of a six-month, face-to-face recertification interview requirement in early FY 2012 (see Figure 1). The new rules were intended to limit ineligible people from participating in Alliance ‘ especially non-District residents ‘ but the drastic enrollment decline suggests the rule is affecting eligible residents’ ability to enroll.
The Alliance recertification requirement is far more burdensome than in other health or social service programs in the District. For example, DC’s Medicaid program requires only annual renewal and does not require participants to interview face-to-face with government staff (documentation can be sent in via mail). Beginning in 2014, eligibility and enrollment in the Medicaid and other social programs will also be conducted electronically via the DC Access System, which streamlines access to multiple public benefits through one point of entry.
The frequent in-person recertification can make it difficult for eligible residents to enroll and maintain eligibility for Alliance, especially working individuals under strict time constraints. National research suggests that when application or recertification processes become more challenging, participation among eligible participants can drop sharply. In addition, community-based organizations and health care providers report that their clients have experienced increased wait-times when recertifying in-person for Alliance, due in part to limited staff available to conduct interviews and even fewer bilingual staff needed to meet the unique language needs of the Alliance population.
Two strategies can address these barriers to participation among eligible residents, while also limiting the ability of non-residents to participate. First, in the short term, a portion of the $2 million cut from the Alliance could go to enhancing staffing for recertification at service centers. The funding can help ensure there are enough staff, reasonable office hours, and needed foreign language competence among interviewers.
Second, as the Alliance is added to the DC Access System, Alliance’s recertification should be streamlined to match the annual renewal requirements of other health care programs. DC Access’s integrated eligibility system, with connections to data sources that can be used to verify residency electronically, will make it easier for eligible residents to recertify without creating a risk of ineligible people getting assistance. It also would reduce the number of times participants need to visit service centers, which would free up staff for more complicated eligibility determinations.
To print a copy of today’s blog, click here.
