The District will soon enjoy large health care savings as the federal government pays for more people and more services, and these should be reinvested to expand health services and improve quality. Instead, the proposed fiscal year (FY) 2016 budget would use those savings to cover gaps outside of health. That is a lost opportunity and not what was intended when the federal government increased health spending under the Affordable Care Act.
The federal government will now pay the full costs for residents who are newly eligible for Medicaid, like childless adults under 200 percent of the poverty line. They will also fully cover the costs of the Children’s Health Insurance Program. 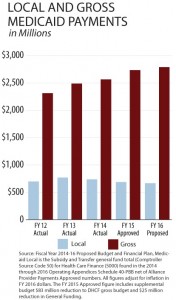 Beyond this, DC will soon use Medicaid to provide substance abuse services for adults. That brings more federal money and more services — and saves DC a lot of money!
Beyond this, DC will soon use Medicaid to provide substance abuse services for adults. That brings more federal money and more services — and saves DC a lot of money!
But the proposed budget would use these savings to cover gaps elsewhere. The budget also would take $23 million from the Healthy DC Fund — which is used to help fund Medicaid and Alliance — to cover non-health expenses.
DC should instead use these funds to expand health care access and quality by:
- Eliminating restrictive rules that contributed to 10,000 people losing coverage from the Healthcare Alliance. The Alliance serves people who are not eligible for Medicaid or Medicare. Rules adopted in recent years require participants to have a face-to-face interview every 6 months to maintain eligibility. This is an undue burden on eligible residents, many of whom have jobs, and up to 67 percent of Alliance re-certifications are terminated because participants are unable to meet it. The Department of Health Care Finance acknowledges the problem, but expresses concerns about the costs of changing it. Savings and the Healthy DC fund could be used to pay for those costs.
- Improving Personal Care Services: The FY 2016 budget proposes reducing reimbursements to companies providing personal care aides for residents with long-term disabilities and other chronic conditions. At the same time, aides are supposed to get a pay increase up to the living wage — $13.50 per hour. If the reimbursement rate reduction makes it hard for companies to pay the living wage, DC could use health savings to set rates at appropriate levels to make that possible.
- Improving Managed Care: Managed Care Organizations serve 175,000 Medicaid beneficiaries, but have had trouble providing case management and care coordination. As a result, they spent $35 million on expenses related to avoidable ER visits, hospital admissions and readmissions — all signs of poorly managed health. DC could use savings for increased oversight and monitoring of the program. The District also could use the funding to develop programs that pay MCOs based on performance — with lower rates for bad outcomes.
The DC Fiscal Policy Institute will testify tomorrow at the Department of Health Care Finance’s budget oversight hearing on these issues. To read the full testimony, click here.
To print a copy of today’s blog, click here.
