Chairman Gray and other members of the committee, thank you for the opportunity to testify today. My name is Jodi Kwarciany and I am a Policy Analyst at the DC Fiscal Policy Institute. DCFPI engages in research and public education on the fiscal and economic health of the District of Columbia, with a particular emphasis on policies that affect low- and moderate-income residents. I am also a member of the DC Medical Care Advisory Committee, a forum for participants and stakeholders in the Medicaid program.
I am here today to speak in support of the FY 2018 budgets of both the Department of Health Care Finance and the Health Benefit Exchange Authority, which help provide critical access to health care coverage and services for thousands of District residents. I also want to share areas where I believe both agencies may improve access to services and ensure better health outcomes.
Department of Health Care Finance
DC continues to lead the way in implementing health reform, and in no small part because of the work of DHCF. Whether it’s expanding Medicaid eligibility beyond federal requirements, creating two Health Home programs that coordinate care for Medicaid beneficiaries with chronic health conditions, or instituting performance metrics in Medicaid managed care contracts, the department has embraced many elements of health reform that will further improve access to coverage and health outcomes while making good use of the District’s dollars. This is further reflected in our uninsured rate of just 3.8 percent, one of the best rates in the country. At the same time, amidst the uncertainty we’re now seeing at the federal level with respect to Affordable Care Act repeal, DHCF has been an instrumental partner in understanding, analyzing and communicating what possible changes could mean for the District. For all these reasons, DHCF should be commended for their work.
Amidst these strong successes, DCFPI and a coalition of other organizations and providers remained concerned that the eligibility process for the DC Healthcare Alliance program creates unnecessary barriers that keep thousands of residents from getting regular and preventive care. We urge the Council to change the program’s six-month in-person eligibility requirement through the FY 2018 budget to ease access to care for eligible residents.
The requirements that all beneficiaries renew their benefits every six months instead of annually, and complete a face-to-face intervie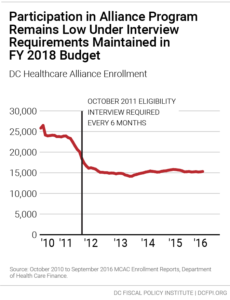 w at ESA service centers at the time of application and for each renewal led to a rapid decline in enrollment in one year after the October 2011 implementation. Enrollment declined by roughly 10,000 beneficiaries, and now stands at about 15,300.
w at ESA service centers at the time of application and for each renewal led to a rapid decline in enrollment in one year after the October 2011 implementation. Enrollment declined by roughly 10,000 beneficiaries, and now stands at about 15,300.
We’ve identified four problems with the current policy:
- It’s hard for eligible beneficiaries – especially those who work and/or have young children – to maintain their benefit. The renewal requirement leads to a large volume of people coming into ESA service centers, who may arrive hours beforehand to stand in line. Often, beneficiaries must go several times to complete one re-certification. And even for those who do secure coverage, we know that at the six-month period, about 33 percent do not re-apply. That’s many individuals who are not receiving regular care.
- It affects the health of DC residents and costs DC money. The requirement appears to have a direct impact on health costs in the program, as many residents avoid regular care and only sign up for the Alliance when they are in high medical need. Per-member monthly costs for Alliance members grew by 22 percent in just one year, compared to a corresponding 6 percent increase for adults in our Medicaid program. For those who are going without coverage entirely, we have to be conscientious of the costs we’re potentially shifting to our emergency rooms.
- It is operationally troublesome for Department of Human Services. As mentioned, the added volume at service centers puts a strain on the DHS, and a study conducted by DCFPI and the Legal Aid Society of the District of Columbia in 2014 found that Alliance beneficiaries make up 25 percent of service center traffic, even though they represent a small number of beneficiaries who get services there. While DHS is working hard to implement an extensive business process redesign initiative that will no doubt alleviate some of this congestion and streamline processes, we remain concerned about the deterrence this has already caused.
- It sends mixed signals to individuals of immigrant status about their place in the community. The District has long been known as a welcoming city for immigrants, including its designation as a Sanctuary City. However, it is difficult to encourage immigrants to take advantage of programs like Alliance when the District imposes additional barriers to their participation. Some beneficiaries have described the enrollment process with words like confusing, intimidating, discriminatory, and inflexible. What’s more, the uninsured rate for DC’s undocumented immigrants in particular stands at 13.4 percent, or about three and a half times our District-wide average of 3.8 percent, meaning we are still not reaching many eligible individuals.
DCFPI is encouraged that two pieces of legislation recently introduced in the DC Council, one by you Chairman Gray, would improve access to the Alliance. One bill would allow Alliance beneficiaries to recertify over the phone or at a community health center, and one of the bills would expand the recertification period back to 12 months. Both of these bills hold promise of eliminating barriers to accessing health care coverage through the Alliance.
We hope that the key provisions of these bills can be incorporated into the FY 2018 budget: switching the recertification period to a year, and allowing health centers where beneficiaries often have established relationships, to help with applications and renewals. DHCF has previously estimated that these changes would cost about $14.9 million per year. Possible sources of funding for a policy initiative like this could include realized savings in managed care expenses as the District continues monitoring and assessing health plan performance and pay-for-performance initiatives.
If the DC Council cannot find other ways to fund this investment, the Council should delay or eliminate the $40 million in estate tax and business tax cuts slated for 2018. DC’s business income taxes are already aligned with Maryland and Virginia, so lowering them will do little to attract thriving businesses, especially compared to investing in a healthy workforce. Eliminating taxes on estates worth up to $5.5 million will do little to attract or retain those few eligible families, whereas a quality health care will improve the lives of thousands.
We applaud the efforts DHCF has taken in understanding Alliance trends over the last year, and hope to continue working with the agency on identifying policy alternatives that would balance legitimate program integrity concerns with respect for the needs of eligible District residents.
HBX
The Health Benefit Exchange Authority has also been, and will continue to be, a key partner in implementing components of health care reform, having served nearly 312,000 individuals since opening. This includes 43,177 DC residents enrolled in private coverage, 80,552 enrolled through the small business marketplace (SHOP), and 187,894 residents who have been found eligible for Medicaid. Although some marketplaces across the country had expensive starts due to the large costs involved up front for technology and consumer assistance, DC Health Link has been able to reap the benefits of its investments, including a first of its kind state partnership with Massachusetts where it will be providing the technology and operational support for their SHOP marketplace, and being recently recognized as the top exchange marketplace in the country for its consumer comparison shopping tools.
HBX’s FY 2018 budget reflects multiple realized programmatic cost savings after prior investments in technical infrastructure. Even with a 20 percent reduction from FY 2017, this budget maintains the funding needed for the agency’s operations for DC Health Link, including information technology (IT) operations, consumer assistance, which take the largest shares.
Yet political uncertainty at the federal level once again affects the quality work that health-based agencies are able to do in the District, and for this reason I recommend that the Exchange continues to hold reserves. The Exchange was notable for having been the first in the nation to create a formalized reserve policy, and should be applauded for partly funding its operational reserve. However, it has further to go to fully meet reserve standards.
Much could change in the coming months – and we need to be prepared as much as possible. Maintaining our local exchange and having a central source for people to find their coverage options and enforce the idea that their health is important is vital.
Conclusion
Within the District, we continue to provide a continuum of coverage options – for all ages, citizenship statuses and income levels, reinforcing this idea that whoever you are, there are health coverage options for you and that your health is important. This could not be achieved without the excellent work of DHCF and HBX, and DCFPI supports these efforts heading into FY 2018.
Thank you for the opportunity to testify, and I am happy to answer any questions.
