Serious glitches in DC’s Medicaid application system have left thousands of DC residents waiting for a Medicaid application to be approved. Another glitch will soon result in the temporary shut-down of a process that allowed 37,000 households to renew Medicaid eligibility last year without having to fill out paperwork or visit a social services office. Until it is fixed, residents will have to complete a complex paper form and bring it in person to one of DC’s social services centers. Undoubtedly, some will not get through the system and will lose health insuranc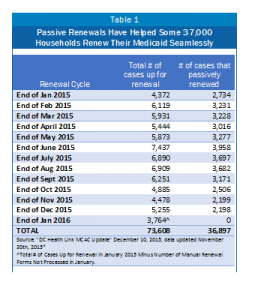 e.
e.
In addition to affecting Medicaid, this will create overwhelming crowds at DC’s social service centers, which already suffer from long lines and paperwork that gets lost frequently. This will create problems for residents seeking other benefits, like SNAP.
These problems are unfortunate in a city that has made health insurance available to most residents and that set up a health care exchange that has helped thousands of residents get affordable health care coverage. DC’s health officials should move quickly to create temporary ways to work around the tech issues, limit the risk of residents losing coverage, and reduce the need to do paper work and in-person visits to the service centers.
Upgrades to the District’s outdated computer system for Medicaid and other public benefits have allowed Medicaid beneficiaries to go through the annual eligibility process without filling out paper work or coming into a service center. These “passive” renewals started in January 2015, and about half of beneficiaries have been able to renew their coverage passively through this process (See Table 1). Not surprisingly, passive renewals are an important way to ensure residents maintain their health coverage. Of the residents who were not able to go through passive renewal this year, about three in 10 failed to maintain their coverage (see Table 2). Some eligibility forms are never returned, but others are lost in the mail, lost at the service center during processing, or stuck in the computer system.
However, a technology glitch in the system will not allow any passive renewals to continue until late next spring. Starting in January, anyone who wants to renew their Medicaid benefits will have to review and complete a 14-page form. Another technological glitch will prevent Medicaid beneficiaries from renewing their benefits online, which means that they will have to mail, fax or hand in person their paperwork at a service center. That’s about 3,765 families or individuals who will need to come into a service center in January (see Table 2). Another 3,500 or so cases that applied for the first time through DC Health Link last year, will also need to come in — meaning ESA will face more than 7,000 renewals. It is unknown how long passive renewal and online renewals will be suspended; the agency has estimated that the problem could be fixed as early as February and as late as the end of the spring.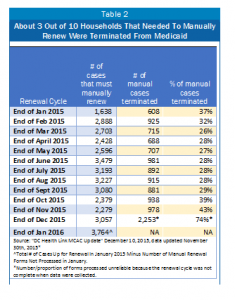
That means that the Economic Security Administration (ESA), which manages the service centers, will see a large uptick in the number of people and amount of paperwork coming in. In the past, influxes of paperwork and people at ESA have led to:
- Client confusion, especially since many have not had to renew in person over the last two years.
- Long wait and processing times at the service centers. This is particularly true for programs and service centers that deal primarily in paper — like the Healthcare Alliance program at Taylor Street service center.
- Unsecure and lost documents during processing at service centers.
- Wrongful termination of benefits and gaps in health coverage.
Beyond the problem with passive renewals, about 2,000 recent applications have not been processed within the required 45-day period, as a result of a technology glitch that scrambles an applicant’s information. Another 2,500 people are affected by a complicated system performance issue affecting their application. This means that at least 5,000 people have been unable to access Medicaid coverage while they wait for a decision on their applications. While all of these applications have been pending for at least 45 days, some have likely been pending much longer’as far back as spring of 2015 when the backlog was discovered or even longer. The underlying problems that cause these glitches will not be fixed until March 2016, so new applications could be affected as well.
The District should take steps now to work around these technology problems — which are inevitable in a big IT rollout — to ensure that those eligible for Medicaid keep and maintain their health coverage:
- The District should not terminate anyone’s Medicaid benefits until the IT platform can once again handle passive renewals and there are online renewal options. DC must act quickly to clear the backlog of applications to ensure that new applicants can get access to care.
- The District should eliminate unnecessary eligibility requirements in other public benefit programs that increase traffic at ESA — including the DC Healthcare Alliance six-month face-to-face interview requirement. Data show that the requirement is a huge barrier to keeping eligible residents enrolled and unnecessarily increases foot traffic at service centers.
- The District should enlist community health centers more in the eligibility and enrollment process. Getting more of the process done outside of the service centers will limit congestion and processing problems.
To print a copy of today’s blog, click here.
