Burdensome application rules in one of the District’s key health insurance programs, the Healthcare Alliance, have led many residents to lose their health insurance and go without needed care. It is a blemish on the city’s otherwise national leadership in extending health insurance to low-income residents. That’s why the DC Fiscal Policy Institute and other advocates are proposing changes to keep residents on the program and ensure that they get the health care that they need.
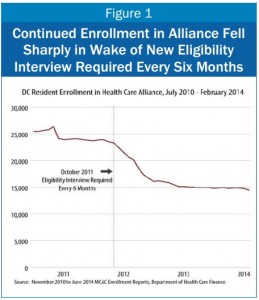
The Alliance provides health insurance to people with incomes below 200 percent of the poverty line and who are not eligible for Medicaid.The District adopted stringent requirements in 2011 — that all Alliance participants recertify every six months through an in-person interview at a service center — and since then enrollment has dropped sharply (see Figure 1). New data from the Department of Healthcare Finance suggests that the six-month interview requirement created a barrier to getting services.
Many eligible residents, especially those who are caring for children and/or have full-time work, are unable to meet the requirement. Beyond that, many families have to make multiple trips to complete their interview, because of a lack of language assistance, long lines, and delays in staff processing information.
The Department of Healthcare Finance asked the community for suggestions to redesign the program. DCFPI, with consensus from other advocates, recommends:
Move from a six-month face-to-face interview to an annual interview. A 12-month recertification period will help Alliance members who must take time off of work to do the interview. It will also help program staff by lessening the number of clients they have to see and improving their ability to assist individual cases.
Allow community health workers to assist with parts of the recertification. If Alliance beneficiaries can complete their recertification with trained Assisters or Community Health workers, the applications will have fewer problems, be processed faster, and reduce the need for multiple trips for one recertification.
Allow Alliance participants to apply online. DC has a new online public benefits system for Medicaid that uses many data sources to verify identity and residency. Yet the Alliance program still uses a paper application. Fully incorporating the Alliance into the electronic application process would mean that many beneficiaries would never need to visit a service center in person.
These changes would prevent eligible residents from unnecessarily losing health insurance, thus building on the city’s commendable efforts to ensure that DC residents have access to health care.
To print a copy of today’s blog, click here.
